30% of People with Depression Don’t Respond to the First Few Antidepressants
Many people with clinical depression have tried an array of medication and still feel sick. Maybe they’ve tried different selective serotonin reuptake inhibitors (SSRIs) or selective norepinephrine reuptake inhibitors (SNRIs). Maybe they’ve taken these antidepressants along with an antipsychotic (a common strategy to boost effectiveness).
Either way, the lack of improvement can make individuals feel even more hopeless and fear the darkness will never lift.
“If this sounds all-too-familiar, you’re definitely not alone. In fact, up to 30 percent of people with depression don’t respond to the first few antidepressants they try.”
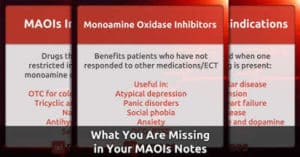
Many individuals with treatment-resistant depression may benefit from a class of antidepressants that today is rarely offered to them: monoamine oxidase inhibitors or MAOIs.
To read the original article posted on PsychCentral.com, click here.
What About Monoamine Oxidase Inhibitors or MAOIs
“MAOIs are the best antidepressants on the planet,” said Mark D. Rego, M.D., a psychiatrist with 23 years of experience, specializing in treatment-resistant individuals, and an assistant clinical professor of psychiatry at Yale University School of Medicine.
Dr. Rego has seen incredible changes in patients with severe depression who were struggling with profound anxiety, insomnia, and suicidal thoughts and taking strong doses of antipsychotic medication and SSRIs. After taking an MAOI, their symptoms “vanished.”
After her husband passed away, Sue Trupin fell into a deep depression that lasted 3 years.
During this time, she tried over 10 different medications in different combinations. She was hospitalized twice.
She received 12 sessions of electroconvulsive therapy. Finally, a new psychiatrist prescribed the MAOI tranylcypromine (Parnate).
As Trupin writes in her eloquent piece, “About 10 days later, sitting in my parked car, I heard on the radio the legendary jazz saxophonist Ben Webster. A shiver of pleasure invigorated me.
Later in the day, I bought bags of fresh food at the market, smiled at a chubby baby, and became overwhelmed by the devotion of a friend. The lights were blinking brightly, and then miraculously they were staying on. I’ve been well now for four years, in my right mind because of an old, inexpensive, and uncommonly prescribed drug.”
“Discovered in the late 1950s, MAOIs have a well-established history of efficacy, particularly in managing difficult-to-treat depression.”
So Why Aren’t MAOIs Prescribed More Often?
For starters, today’s psychiatrists may have less experience with this drug class, said Kristina Deligiannidis, M.D., an associate professor at The Feinstein Institutes for Medical Research at Northwell Health.
In his editorial, Much Ado About Nothing, Australian neuropharmacologist and MAOI expert Ken Gillman, M.D., cites research that’s found this to be true.
Gillman also notes that “the ability to properly manage MAOI treatment should be in the repertoire of all psychiatrists. It is regrettable that this is not the case.”
In fact, Gillman is part of the “International MAOI Expert Group,” which includes clinicians, academics, and researchers.
In this statement, he and his colleagues note that the “group was formed in March 2018 to promote actions aimed at improving education; stimulating research; increasing clinical usage; and assuring the continued availability of MAOIs worldwide.”
While MAOIs aren’t the right choice for everyone, Dr. Deligiannidis noted that they “should be considered part of a comprehensive treatment plan” for individuals with treatment-resistant depression or atypical depression.
She defined atypical depression as “mood reactivity, significant weight gain or increase in appetite, hypersomnia, leaden paralysis, and a long-standing pattern of interpersonal rejection sensitivity.”
There are other reasons MAOI use has declined—reasons that have more to do with misunderstandings than actual facts. Below, you’ll find several common concerns followed by reality.
Concern: Too Restrictive Diet
One of the biggest concerns with prescribing MAOIs is that patients won’t be able to adhere to the stringent diet that’s required.
This means abstaining from foods that are high in the amino acid tyramine because of the danger of a hypertensive crisis (a severe spike in blood pressure that can lead to stroke).
However, today, this stringent diet isn’t actually all that stringent.
According to Rego, “You have to almost go out of your way to get a [hypertensive] reaction.” He gives patients taking MAOIs a simple list of foods that aren’t allowed and foods that are allowed in moderation.
Deligiannidis noted that in the past, some foods that were believed to have high tyramine levels contain little or no tyramine, including raspberries, chocolate, avocadoes, bananas, and Chianti wine.
Plus, as Gillman notes in his editorial, because of recent changes in food production techniques, the once high concentrations of tyramine in foods such as aged cheeses, salami, and soy sauce have significantly diminished.
In fact, today, many matured kinds of cheese—once thought to be dangerous– have negligible concentrations of tyramine, he writes.
Concern: Serotonin Syndrome
Combining certain drugs with MAOIs can cause serotonin syndrome, also known as serotonin toxicity. Serotonin syndrome can range in severity and can be fatal.
Some individuals have mild symptoms, such as increased blood pressure and heartbeat, dilated pupils, sweating, shivering, and twitching muscles.
Others can additionally have hyperthermia, agitation, and frenetic speech. In severe cases, individuals have all of these symptoms, along with muscle rigidity, delirium, and rapid, dramatic swings in pulse rate and blood pressure.
According to Rego, taking the over-the-counter cough suppressant dextromethorphan, along with an MAOI, can cause serotonin syndrome. So can taking an SSRI or SNRI.
Fortunately, these drug interactions are “all easily avoidable,” Rego said. He noted that he’s less concerned about patients making a mistake and more concerned about them going to the hospital where the staff is unaware that they’re taking an MAOI or doesn’t understand how MAOIs work.
To avoid this, he stresses the importance of wearing an alert bracelet or a pendant—just like you would if you had severe allergies or diabetes.
It’s common for individuals to be taking an SSRI or SNRI before trying an MAOI. To avoid serotonin syndrome, it’s important to have a “wash-out” period.
This is when individuals need to wait weeks for their bodies to eliminate a drug before they can start the new one. Understandably, during this time, there’s a concern that depression symptoms will worsen.
Consequently, Rego prescribes medication to help bridge this gap. For example, if a patient is taking Zoloft, he might prescribe a benzodiazepine to manage anxiety, and lithium to manage mood during the 2-week waiting period.
He also recommends patients alert their loved ones about the change and get extra support; make sure they’re getting enough sleep and rest, and keep stressors at bay.
Therapy also is a critical part of a comprehensive plan and could help tremendously during this transition.
Available MAOIs
Rego noted that there are four licensed MAOIs in the U.S. Selegiline (Emsam) is an MAO-B inhibitor, which comes in a skin patch. The other three MAOIs are non-selective.
“Marplan is almost never used [simply because] we’re not that familiar with it,” Rego said. “Nardil is commonly used, but it’s sedating and causes weight gain.”
Rego prefers Parnate and noted that it “should be everyone’s number one choice.” “It’s the easiest to take and doesn’t make you tired or gain weight.”
The only significant side effect, he said, is that it’s stimulating.
This is why whenever he’s prescribing any antidepressants, Rego asks patients how well they can tolerate caffeine.
If they mention adverse reactions (e.g., faster heartbeat, shortness of breath), Rego might prescribe a medication to control anxiety until the stimulating effects wear off.
MAOIs won’t work for everyone. For example, they’re typically contraindicated for people with severe personality disorders.
That’s because, Rego said, these individuals tend to be impulsive, struggle with suicidal thoughts (and attempts), and engage in self-injurious behavior. Which means they can intentionally take a medication that interacts with their MAOI, he said.
However, for some individuals with severe depression, MAOIs can be transformative. As Rego said, “It is not an exaggeration to say, it can change a person’s life.”
And that means physicians must become experts in prescribing MAOIs and offer them as a viable option when other antidepressants haven’t worked.





Recent Comments